Spinal Conditions
Our Conditions
Home>Conditions
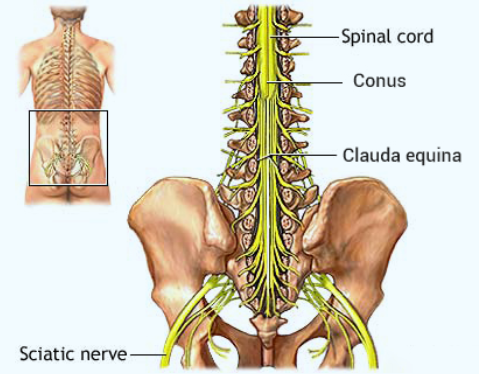
The spine in the lower (lumbar) back consists of the bony vertebrae, discs, nerves and other structures. The vertebrae, which stack up to create the spinal column, surround and protect the spinal cord and nerve roots. The end of the spinal cord (conus) is near the top of the lumbar spine. Below this, the nerve roots hang down in individual strands. These nerve roots, when viewed together, are somewhat similar in appearance to a horse’s tail, so the term used to describe them is cauda equina. The nerve roots travel out small bony windows (foramenae). The discs are located between each vertebra. Discs consist of a fibrous outer layer (annulus) surrounding a gelatinous center (nucleus). They allow motion between vertebrae, act as shock absorbers, and distribute the stress and strain placed on the spine.
Various conditions may be present, due to genetic or developmental problems, disease, trauma, or simply as a result of the normal aging process. These conditions may lead to pain, deformity, or a reduction in the capacity to carry out the usual activities of daily life. The most common condition is arthritis of the spinal joints. This can result in a narrowing of the room available around the nerve roots. This is called stenosis of the spinal canal due to bone spurs, cysts, or other degenerative changes. Another spinal condition that can pinch the nerve roots is slippage of one or more vertebrae on the vertebra below, called spondylolisthesis.
Most patients with stenosis have mild findings and do not experience serious symptoms. Some people, though, may require surgery if the nerve roots are severely irritated or the spinal column becomes unstable. There are rare circumstances in which patients require urgent surgery. These include cauda equina syndrome and/or progressive neurologic loss (increasing weakness). Symptoms of cauda equina syndrome include changes in bowel or bladder function, numbness or change in sensation in the area around the buttocks, genitalia, or thigh, and weakness and/or radiating numbness in the legs. People who develop symptoms of cauda equina syndrome should seek medical attention immediately.
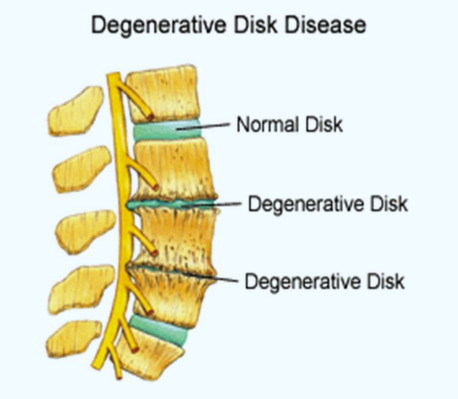
Degenerative Disc Disease:
As we age, the water and protein content of the body’s cartilage and discs change. This change results in weaker, more fragile and thin cartilage. Because both the discs and the facet joints that connect the vertebrae are partly composed of cartilage, these areas are subject to wear and tear over time. The gradual deterioration of the discs is referred to as degenerative disc disease. This can be noted on x-ray tests or MRI scanning of the spine as a narrowing of the normal disc space between the adjacent vertebrae. Degeneration of the disc can cause narrowing of the spinal canal (stenosis) and apply pressure on the nerve roots. This can be experienced as pain which radiates down the thigh and/or leg with walking or standing (neurogenic claudication). If the pressure on the spinal nerve roots continues, numbness or muscle weakness in the leg or foot may develop.
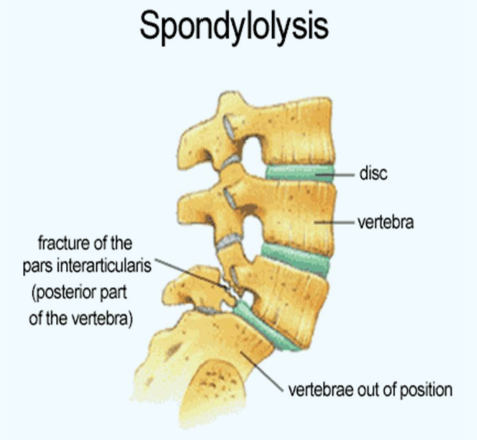
Spondylolisthesis:
Spondylolisthesis may be the result of trauma, degenerative changes, or a developmental crack in one of the vertebrae. Due to the constant forces experienced in the low back this fracture does not usually heal in an adult, but may not produce significant symptoms. Sometimes the cracked vertebra may slip forward over the vertebra below it. This is known as spondylolisthesis. In some people, this slippage can produce pressure on the nerve roots causing symptoms of back and/or leg pain, typically with walking or standing.
Conservative Management: Backache associated with spinal arthritis is common and usually comes and goes without formal treatment. The best prevention and treatment is staying fit and active. For severe episodes of back or leg pain, with the passage of time and treatment with ice, heat, and short periods of rest, inflammation around the nerve roots can resolve on its own. Steroid injections may help relieve the pain by reducing some of the inflammation around the nerves, allowing the irritated nerve time and space to heal. If this conservative care does not relieve symptoms or if there is progressive neurological damage, surgery may be necessary.
Surgery: There are two general types of surgery done for Spinal Stenosis or Spondylolisthesis: decompression (taking pressure off the nerve roots) and fusion. If there is no instability, decompression alone may help nerve pain going into the buttock and legs. If there is significant instability the spine may also need to be fused (surgically stabilized) either from the front (anterior) or back (posterior), or both.
Posterior Spinal Fusion (PSF): is an operation to stabilize the spine, relieve pressure on irritated nerves and ensure this pressure does not return at that place. This surgery involves an incision in the midline of the back (posterior). The spinal surgeon will protect the nerve roots and safely remove the bone spurs, cysts, or other material pressing on the nerve. Next, bone graft is placed along the back of the spine, allowing the two vertebrae to grow together as one (fusion) over some months after surgery. After the operation, the area must be kept somewhat immobile to ensure the fusion occurs. This may be accomplished by activity restriction, the wearing of a soft support brace, or a hard plastic brace. In some patients, metal screws and rods are placed in the spine to hold the bones while the fusion heals.



Interbody Fusion: Through the same incision on your back, the spinal surgeon will then safely remove the degenerated disc between the two vertebrae. Next, a bone graft will be placed between the two vertebrae where the disc had been, allowing the two vertebrae to grow together as one (fusion) over some months after surgery. After the operation, the area must be kept somewhat immobile to ensure the fusion occurs. This may be accomplished by activity restriction, the wearing of a soft support brace, or a hard plastic brace.
The purpose of this surgery is to stabilize the spine and relieve leg/back pain, numbness, weakness, or lack of coordination and motor control caused by pressure on the nerves. The success rate of relieving leg pain is very high.
The surgery typically lasts two or more hours, depending on the number of discs operated upon, whether or not previous surgery has been performed, and the severity of pressure on the nerves. The likelihood of significant blood loss is dependent on the number of levels requiring surgery; if one or two level surgery is needed, blood loss can be minimal so sometimes no blood donations are necessary before the operation. Time spent in the hospital is short—most patients can go home three to five days after the surgery.
Surgery and anaesthesia involve stresses to many organs and tissues in the body. Incisions and handling tissues during surgery can result in many problems. The benefits of surgery must be carefully weighed against these risks. Some more common or serious problems are listed here.
Spinal Cord or Nerve Root Injury: Permanent injury to the spinal cord or nerve roots is extremely rare. It is not unusual, however to experience minor temporary tingling, numbness, weakness or pain which resolves over several weeks. All precautions will be taken but rarely, more serious nerve injuries may occur, effecting walking, balance, bowel or bladder functions.
Failure of fusion: On rare occasions the bone graft does not heal properly. The likelihood of this is greatly increased by smoking or using nicotine of any kind. This can cause the hardware to fail, and the bone graft may shift. In these cases, additional surgery may be needed. For this reason we recommend quitting smoking at least one month before surgery and refraining from smoking for at least 3 months after surgery. Smoking also causes more rapid degeneration of the spine, and continuing to smoke increases the likelihood of requiring treatment at another level of the neck.
Dural Tear: Leakage of spinal fluid can occur due to a tear in the tissue (called the “dura”) holding the spinal fluid and containing the nerves. On rare occasions additional surgery may be needed. Infection: Infection is always a post-operative risk and occurs in approximately 1–2% of surgical patients, varying by surgery type.
Infections may be superficial or deep into the bone. You are given antibiotics before and after the surgery to help prevent this complication. Please follow the instructions for wound care to help prevent infection.
Other complications: Other possible complications include blood clots, pneumonia and complications related to the general anesthesia. Persistent hoarseness and/or swallowing problems may last for several weeks. Please call us if this persists.
Adequate rehabilitation is crucial for a successful result. Many patients with spinal injuries have suffered from spinal pain for some time. This may result in considerable weakening of the spinal muscles due to lack of exercise, so you should return to your normal activities slowly.
The primary form of rehabilitation after surgery is an aggressive walking program. You should start immediately after discharge, walking more and more each day. In general, we recommend two to three episodes of exercise per day. The average patient can be walking 15 minutes twice a day by their first postoperative visit and 30–40 minutes twice a day by six weeks after surgery. Walk more if you are so inclined!
Patients routinely experience a dramatic, remarkable reduction in their back and leg pain; however, of the two the leg pain is more predictably alleviated. If the nerve has been irritated for a long time, then a more gradual reduction of the leg pain is to be expected. As the nerve heals, expect tingling or a warm feeling. Depending on how long the symptoms have been present, strength is usually the second symptom to improve. Numbness in the leg / foot is the last to resolve and, if present for long enough prior to surgery, may be permanent.
Back pain associated with the incision is largely improved within two to three weeks. Increased pain with prolonged sitting and driving is also expected and, for safety reasons, we recommend refraining from driving for approximately three weeks.
At your first post-operative visit we will inspect your wound and remove any stitches as necessary.

Do not soak your wound. No bathtub, swimming, or hot tub, etc. until you have received permission from your physician. Do not remove any “butterfly” bandages right next to your skin. These are designed to get wet and fall off in the shower over time.
To shower: simply remove the outer gauze bandage and shower as usual. Blot the incision dry, and then cover it with a clean, dry bandage.
Prescribed narcotic pain medication may cause some constipation. To help with this:
If you need a refill on your pain medication, please have your pharmacy fax the refill request to our office 1 (888) 636-7840 and please allow up to 48 hours for the request to be processed. Refills on pain medication will not be filled after hours or on weekends or holidays. Be aware of how much pain medication you have, & obtain refills before you run out.
Avoid twisting your neck to the extremes, and avoid forced bending of your neck either forward or backward. Gentle range of motion of the neck is OK. Do not drive until you have received permission from your physician.
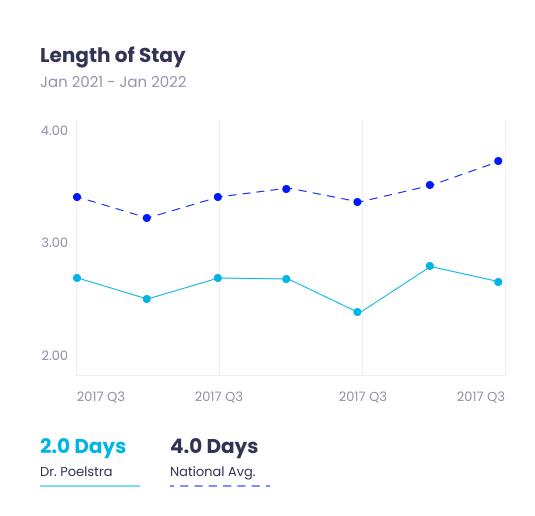
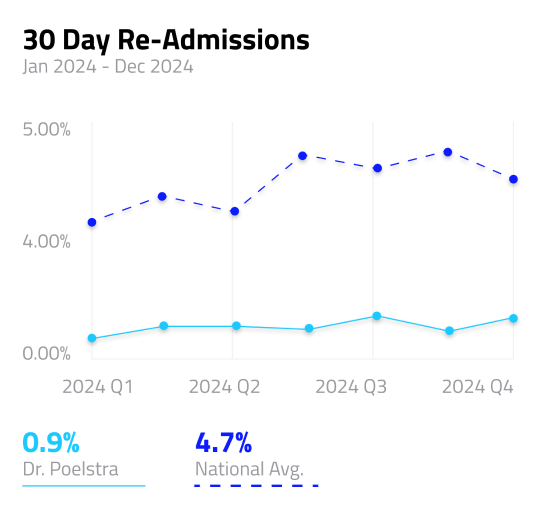
We’re proud to share our results from our outstanding spine surgeries performed to date. Although these results show that the Robotic Spine Institute of Las Vegas provides some of the best spine care and treatment in the world, we are consistently evaluating and improving our methods to treat cervical disc, lumbar spine and other medical conditions in the Las Vegas, Henderson, and North Las Vegas and surrounding areas.

speak with one of OUR TEAM MEMBERS